|
 |
- Search
| J Neurointensive Care > Volume 6(1); 2023 > Article |
|
Abstract
Background
This study aimed to analyze the catabolic phases of patients with traumatic brain injury (TBI) by performing the Nitrogen Balance Test (NB Test).
Methods
This single-centered, retrospective study included data from 292 patients who underwent NB tests from 2019 to 2022 and categorized them as TBI and Non-TBI groups. The basic clinical factors (gender, age, and initial GCS), critical care factors (APACHE, SOFA, and ICU stay days), and outcomes (GOS). The trend of the NB test was investigated in all groups and analyzed the statistical correlation of the NB test was with severity, critical care factors, and outcomes.
Results
A total of 52 patients were found to have TBI. The 26 out of 52 TBI patients underwent the second NB test 1 week after the first NB test. The deficiency of protein calculated was 24.375 g. There was a significant statistical difference of NB test patterns between the non-TBI and TBI patients.
Many patients fall into the catabolic phase in intensive care units1-2). In critically ill patients, stress hormones and inflammatory mediators are activated, and metabolically, proteolysis by catabolic action occurs. Especially, in stressful situation such as post trauma status, more reactions are induced by stress, ultimately leading to catabolic effects. The main metabolic change in response to injury that leads to a series of reactions is the reduction of the normal anabolic effect of insulin. After trauma, free fatty acids and triglycerides are consumed such as primary sources of energy. At the same time, proteolysis leads the negative nitrogen balance. When this catabolic phase is severe, many patients tend to have a poor prognosis3-9). This trend applies to critically ill and neurological critically ill patients10). Neurological critically ill patients also have higher morbidity and mortality if insufficient nutrient supply is poor11-13). So, proper nutrition supply in the catabolic phase such as early enteral nutrition at a proper time is very important. Despite the importance of the catabolic phase, there are only a few studies on catabolic trends neurotrauma patients exhibit over time after injury. There are many tests that can determine the degree of catabolic phase, but in practice, the nitrogen balance test (NB test) is the most commonly used14-23). So we investigated the trends of catabolic phase in head trauma patients and the difference from other neurologically critical patients by using NB test.
This study included patients expected to be admitted to the neurological intensive care unit (NCU) for >1 week from June 2019 to March 2021. In principle, the treatment protocol of the intensive care unit of this hospital is to perform the NB test once a week. However, NB tests were not performed for patients with renal failure, those who started eating by mouth instead of L tube and found it difficult to calculate intake, those whose caregivers refused active treatment, and those who were abruptly discharged or transferred to general hospital rooms.
All patients were classified into two groups: trauma and non-trauma (Tumor and stroke). Basic clinical factors, such as age, sex, mortality, height, weight, BMI, and other factors were examined in all patient groups. Additionally, initial GCS, initial Apache score, NCU check-in period, SOFA score, NB test results (at the time of admission, 1-week later, and 2-weeks later) and the GOS at 3 months later were investigated.
We then first analyzed whether there was a significant change in the trend of the NB test statistically. We then analyzed the NB test, trauma, initial GCS, initial Apache score, NCU admission period, SOFA score, and GOS at 3 months later.
Statistical analysis was performed using SPSS Statistics 25.0 (IBM, Chicago, USA). Fisher exact tests or χ2 tests were performed for categorical variables, while independent t-test for continuous variables of clinical factors. A p-value <0.05 was considered statistically significant. All data are presented as mean ± standard deviation for continuous variables.
A total of 3,768 patients were admitted to the NCU during the study period. Among these neuro-surgical patients, 292 neuro-critically ill patients were included in the final analysis. Among the 292 patients, the number of TBI patients was 52. Among the 240 non-trauma patients, 105 had brain tumor-related diseases, 111 had stroke, and 24 had other diseases, such as seizure, wound infection, and sepsis. The proportion of men in trauma patients was higher than that in non-trauma patients, and the proportion of younger age in trauma patients was higher than that in non-trauma patients statistically. The initial GC and APACHE scores reflecting severity did not show a statistically significant difference (Table 1).
Of the 292 patients, 160 completed the second NB test and 79 completed the third NB test. Analysis of NB test trends in all group shows -6.77 ± 4.9 g/d in the first NB test, -7.24 ± 5.1 g/d in the second NB test, and -4.3 ± 5.3 g/d at 2 weeks follow-up. This study found that the NB test did not improve until >2 weeks after admission to the NCU (Fig. 1). Next, the authors analyzed NB test trends by dividing them into traumatic and non-traumatic groups (Fig. 2). The first NB test was -7.1 g/d in the trauma group and -7.3 g/d in the non-traumatic group, with no statistical difference. However, in the second NB test, there was a statistical difference in the NB test results of the non-traumatic and traumatic groups. In the non-traumatic group, the second NB test value was –7.2 g/d, which was not significantly changed compared to first NB test, but in the trauma group, the second NB was -11.2 g/d, which was significantly lower than 1st NB (p = 0.005) (Fig. 2). In the third NB test, the traumatic and non-traumatic groups showed a slight deviation from the catabolic phase with -4.7 g/d -4.2 g/d, respectively.
We analyzed the input and output of the second NB test to determine the causes of increased negative NB tests in the trauma group (Fig. 3). As a result, even though the input increased from 8.06 to 11.07, the NB test value became more negative because the output increased a lot. Thus, it can be seen why the second NB test in TBI group value became more negative was not because of decreased input, but because of increased output.
We also analyzed the correlation between NB test and severity and outcome factors. Severity was evaluated as the initial GCS, SOFA, and APACHE score, and the outcome was evaluated as ICU tenure and GOS at 3 months later. As a result, our NB test did not demonstrate a statistical correlation between severity and outcome (Table 2).
This study divided the NCU patients into traumatic and non-traumatic groups to investigate trends in NB tests. The results showed that the catabolic phase was increased on the second NB test, that is, the NB test 1 week after the trauma, in the head trauma patient group. It was not until 2 weeks later that we observed improved catabolic phase. The catabolic phase in ICU patients has already been reported in many prior studies24-28). The most reliable test for determining at this catabolic phase may be the NB test24,29-35).
This study analyzed the worsening of the second NB test in patients with TBI. As a result, it was confirmed that the NB test worsened due to an increase in protein output, rather than a decrease in the input or nutrition supply. This worsening of the catabolic phase on the NB test of the second phase can have various causes. For examples, sedation, targeted temperature management, and multiple operations can worse the catabolic phase. When coma therapy or body temperature is lowered, caloric requirements tend to decrease36). In patients with unstable vital signs, nutrition may not be absorbed in the intestine even if it is supplied. We performed coma therapy and target temperature management for ICP control in patients with severe brain injury. About 1 week after admission, this treatment should end; thus, the NB test may appear as the catabolic phase. Therefore, further study should be conducted for correcting surgical and intensive care factors.
This study should be of interest because the nutrition-related data was carefully collected because it was a protocol base study, which was consistent with treatment protocols because it was conducted in a single institution, and through multidisciplinary rounds. In addition, nutrition-related data was measured daily by a clinical dietitian during multidisciplinary rounds, and other SOFA and Apache scores were automatically measured. However, further large, prospective studies with surgical factor correction and multiple intensive care factor corrections should be conducted in the future.
This study had limitations. First, there were high dropout rates. Second, this was a single-centered study with few participants. Third, this was retrospective study. The 292 of of 3,700 patients, or <10 %, have been introduced, which is likely to result in the omission of very severe cases. In particular, due to the law of discontinuation of life-sustaining treatment, there is a tendency to miss a lot of serious illness because caregivers give up treatment early. Finally, many patients tend to be missing when renal function declined because it was an NB test study. Thus, there may also be cases where the catabolic phase was clearly present but were missing.
For many critically-ill patients, especially the head trauma group, the NB test accurately showed more severe catabolic phase than the non-traumatic group. Therefore, actively managing the catabolic phase by attempting to improve the NB test through protein supply from the beginning should be practiced in head trauma patients.
Fig. 1.
Trends of nitrogen balance test (NB test) in all participants. The initial NB tests revealed the catabolic phase of the patients. And it sustained until the 2nd NB test. The catabolic phase was recovered at 3rd NB tests, it was performed at 2weeks later.
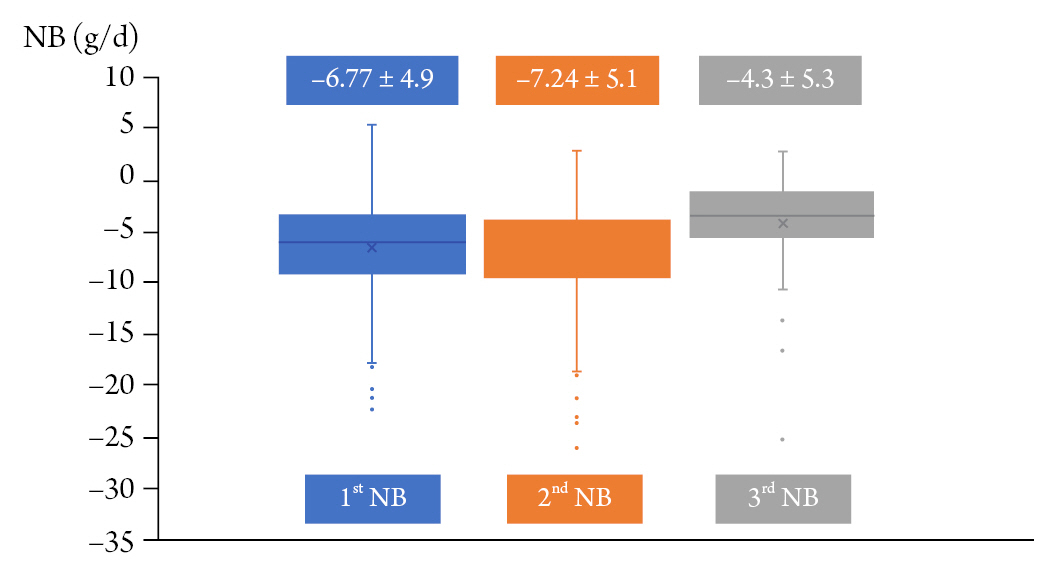
Fig. 2.
Nitrogen balance test (NB test) results according to the presence of trauma. In the TBI groups, 2nd NB test was revealed that the catabolic phase was worsened. In contrast, in the non-traumatic group, the 2nd NB test did not differ significantly from the 1st NB test. Both 3rd NB tests showed improvement in the catabolic phase.
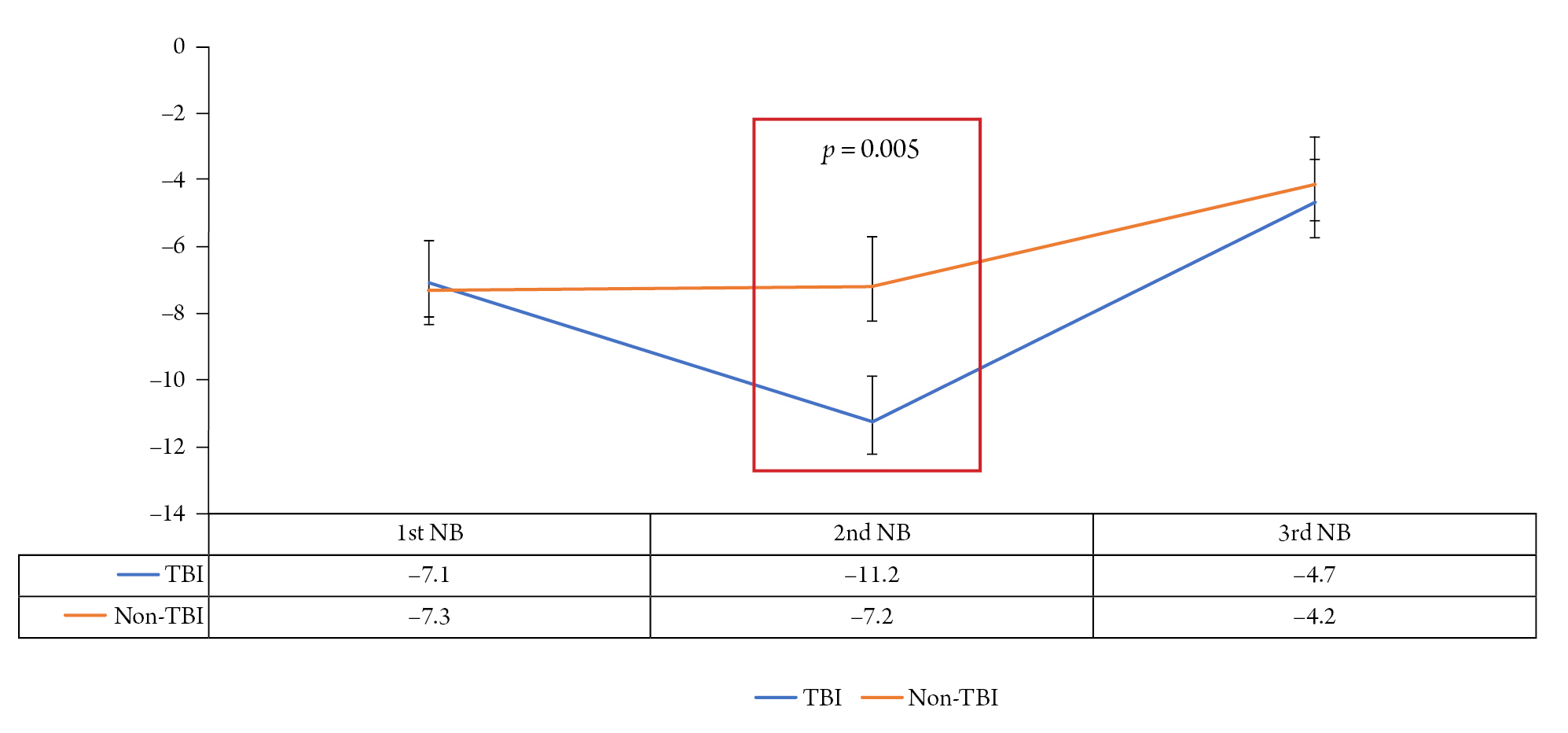
Fig. 3.
Analysis of first and second nitrogen balance test (NB test) in TBI group, focused on the input and output. Compared to the time of the first NB trial, it can be seen that the diet supply in patients has increased. However, even though the input increased, the output increase was much higher, and the overall negative was worse in the second NB test. However, it can be seen that the cause of the second NB test in TBI group is not because intput is reduced, but because output is increased.
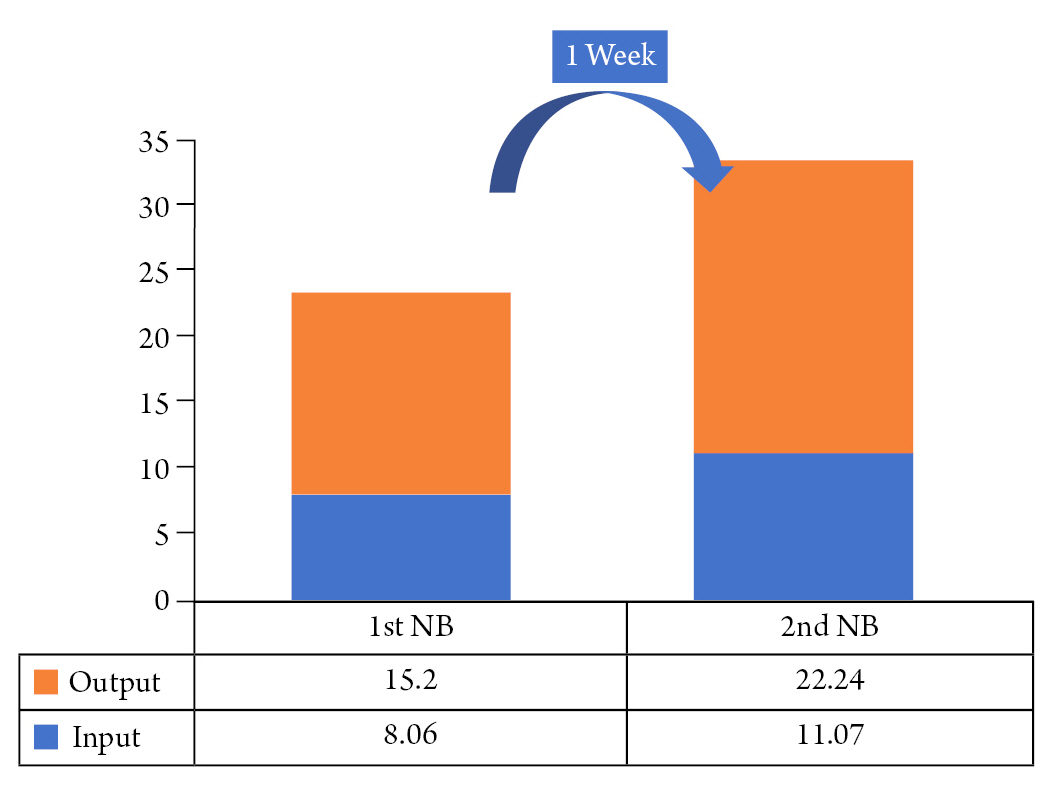
Table 1.
Baseline characteristics of patients according to the presence of trauma
| Patients of TBI | Patients of Non-TBI | p-value | |
|---|---|---|---|
| Sex (Percentage of men) | 77.6 | 32.7 | 0.016* |
| Age (years) | 60.7 | 65.7 | 0.04 |
| Height (cm) | 163.8 | 160.7 | 0.41 |
| Weight (kg) | 66.02 | 68 | 0.35 |
| BMI (kg/m2) | 22.9 | 25.1 | 0.23 |
| Initial GCS | 8.9 | 9.3 | 0.59 |
| Initial APACHE | 18.6 | 16.5 | 0.36 |
REFERENCES
1. Rosenthal MD, Bala T, Wang Z, Loftus T, Moore F. Chronic critical illness patients fail to respond to current evidence-based intensive care nutrition secondarily to persistent inflammation, immunosuppression, and catabolic syndrome. JPEN J Parenter Enteral Nutr 2020;44:1237–1249.




2. Dai GL, Ferrando AA, Lee SW, et al. Evidence for a critical step activating muscle proteolysis in catabolic patients. J Am Soc Nephrol 2003;14:330a–30a.
3. Chen Y, Yang X, Zhu Y, Zhang X, Ni J, Li Y. Malnutrition defined by geriatric nutritional risk index predicts outcomes in severe stroke patients: a propensity score-matched analysis. Nutrients 2022;14:4786.



4. Shaikh A, Khrais A, Le A, Ahlawat S. Malnutrition imparts worse outcomes in patients with diverticulitis: a nationwide inpatient sample database study. Cureus 2022;14:e26973.



5. Matsui R, Rifu K, Watanabe J, Inaki N, Fukunaga T. Current status of the association between malnutrition defined by the GLIM criteria and postoperative outcomes in gastrointestinal surgery for cancer: a narrative review. J Cancer Res Clin Oncol 2023;149:1653–1643.


6. Rim DS, Kaye AJ, Wang WZ. Malnutrition is associated with worse outcomes of inpatient endoscopic retrograde cholangiopancreatography. Cureus J Med Science 2022;14:e26253.



7. Sousa IM, Burgel CF, Silva FM, Fayh AP. Prognostic value of isolated sarcopenia or malnutrition-sarcopenia syndrome for clinical outcomes in hospitalized patients. Nutrients 2022;14:2207.



8. Wham C, Curnow J, Towers A. Malnutrition risk: four year outcomes from the health, work and retirement study 2014 to 2018. Nutrients 2022;14:2205.



9. Goins EC, Weber JM, Truong T, Moss HA, Previs RA, Davidson BA, et al. Malnutrition as a risk factor for post-operative morbidity in gynecologic cancer: analysis using a national surgical outcomes database. Gynecol Oncol 2022;165:309–316.


10. Zhu YB, Yao Y, Xu Y, Huang HB. Nitrogen balance and outcomes in critically ill patients: a systematic review and meta-analysis. Front Nutr 2022;9:961207.



11. Caliri S, Andaloro A, Corallo F, Donato A, Marino S, Mantarro C, et al. Recovery of malnutrition in a patient with severe brain injury outcomes: a case report. Medicine (Baltimore) 2019;98:e16755.


12. Baltazar GA, Pate AJ, Panigrahi B, LaBoy S, Prosniak R, Mody A, et al. Malnutrition as measured by albumin and prealbumin on admission is associated with poor outcomes after severe traumatic brain injury. Am Surg 2015;81:E61–E63.



13. Prosser-Loose EJ, Smith SE, Colbourne F, Paterson PG. Can the influence of pre-existing protein-energy malnutrition (PEM) on outcome from brain ischemia be reliably studied with the rat 2-vessel occlusion (2-VO) model? Stroke 2010;41:E484–E84.
14. Gupta M, Sharma RK, Rastogi A, Varun TK, Bala S, Saharan V. Effect of plane of nutrition on nitrogen balance, blood biochemical and serum enzymes in goats. Indian J Anim Res 2018;52(11):1603–1607.


15. Dong ZY, Shi N, Gao XR. Effect of early enteral nutrition support on nitrogen balance and NIHSS score in elderly patients with acute cerebral stroke and dysphagia. Pteridines 2018;29:91–96.

16. Kumagai H, Baral BR, Shiino T, Devkota NR, Oishi K, Hirooka H, et al. Effects of plane of nutrition on growth, feed intake, digestibility and nitrogen balance in Murrah graded male buffalo (Bubalus bubalis) calves in Nepal. Anim Sci J 2012;83:50–54.


17. Zessner M, Thaler S, Ruzicka K, Natho S, Kroiss H. Considerations on the importance of nutrition habits for the national nitrogen balance of Austria. Water Sci Technol 2010;62:21–27.



18. Sanz París A, Lázaro J, Guallar A, Gracia P, Caverni A, Albero R. Nutrición enteral continua frente a nutrición en bolo: efectos sobre el péptido C urinario y el balance nitrogenado [Continuous enteral nutrition versus single bolus: effects on urine C peptide and nitrogen balance]. Med Clin (Barc) 2005;124:613–615.

19. Boulétreau P, Chassard D, Allaouchiche B, Dumont JC, Auboyer C, Bertin-Maghit M, et al. Glucose-lipid ratio is a determinant of nitrogen balance during total parenteral nutrition in critically ill patients: a prospective, randomized, multicenter blind trial with an intention-to-treat analysis. Intensive Care Med 2005;31:1394–400.



20. Albers MJ, Steyerberg EW, Hazebroek FW, Mourik M, Borsboom GJ, Rietveld T, et al. Glutamine supplementation of parenteral nutrition does not improve intestinal permeability, nitrogen balance, or outcome in newborns and infants undergoing digestive-tract surgery: results from a double-blind, randomized, controlled trial. Ann Surg 2005;24:599–606.
21. Briassoulis G, Tsorva A, Zavras N, Hatzis T. Influence of an aggressive early enteral nutrition protocol on nitrogen balance in critically ill children. J Nutr Biochem 2002;13:560.


22. Mauldin GE, Reynolds AJ, Mauldin GN, Kallfelz FA. Nitrogen balance in clinically normal dogs receiving parenteral nutrition solutions. Am J Vet Res 2001;62:912–920.


23. Taylor SJ, Fettes SB. Enhanced enteral nutrition in head injury: effect on the efficacy of nutritional delivery, nitrogen balance, gastric residuals and risk of pneumonia. J Hum Nutr Diet 1998;11:391–401.

24. Eden T, McAuliffe S. Critical care nutrition and COVID-19: a cause of malnutrition not to be underestimated. BMJ Nutr Prev Health 2021;4:342–347.



25. Barcus GC, Papathakis PC, Schaffner A, Chimera B. Nutrition screening, reported dietary intake, hospital foods, and malnutrition in critical care patients in Malawi. Nutrients 2021;13:1170.



26. Zamora-Elson M, Martinez-Carmona JF, Ruiz-Santana S. Recommendations for specialized nutritional-metabolic management of the critical patient: consequences of malnutrition in the critically ill and assessment of nutritional status. Metabolism and Nutrition Working Group of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC). Med Intensiva (Engl Ed) 2020;44 Suppl 1:19–23.


27. Chisti MJ, Salam MA, Ashraf H, Faruque AS, Bardhan PK, Hossain MI, et al. Clinical risk factors of death from pneumonia in children with severe acute malnutrition in an urban critical care ward of Bangladesh. PLoS One 2013;8:e73728.



28. Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet 2013;113:1219–1237.


29. Danielis M, Lorenzoni G, Cavaliere L, Ruffolo M, Peressoni L, De Monte A. Optimizing Protein Intake and Nitrogen Balance (OPINiB) in adult critically iii patients: a study protocol for a randomized controlled trial. JMIR Res Protoc 2017;6:e78.



30. Dickerson RN. Nitrogen Balance and Protein Requirements for Critically Ill Older Patients. Nutrients 2016;8:226.



31. Fernández R, Urbano J, Carrillo Á, Vivanco A, Solana MJ, Rey C, et al. Comparison of the effect of three different protein content enteral diets on serum levels of proteins, nitrogen balance, and energy expenditure in critically ill infants: study protocol for a randomized controlled trial. Trials 2019;20:585.




32. Kand D, Dickhoefer U. The effects of rumen nitrogen balance on nutrient intake, nitrogen partitioning, and microbial protein synthesis in lactating dairy cows offered different dietary protein sources. J Dairy Sci 2021;104:4223–4235.


33. Moizé V, Pi-Sunyer X, Vidal J, Miner P, Boirie Y, Laferrère B. Effect on nitrogen balance, thermogenesis, body composition, satiety, and circulating branched chain amino acid levels up to one year after surgery: protocol of a randomized controlled trial on dietary protein during surgical weight loss. JMIR Res Protoc 2016;5:e220.



34. Scheinin M, Junnila J, Reiner G, MacDonald A, Muntau AC. Nitrogen balance after the administration of a prolonged-release protein substitute for phenylketonuria as a single dose in healthy volunteers. Nutrients 2021;13:3189.



- TOOLS
-
METRICS

-
- 0 Crossref
- 1,628 View
- 38 Download
- Related articles in JNIC
-
Cardiac Arrest in Traumatic Brain Injury ;0()
Analysis of Prognostic Factors in Patients with Hemorrhagic Moyamoya Disease2023 April;6(1)
Locked in Syndrome After Penetrating Traumatic Brain Injury2023 April;6(1)