Allergic Reaction Induced Brainstem Stroke in a Patient With Moyamoya Disease: A Case Report
Article information
Abstract
A patient who ate peaches and developed urticaria complained of left sided weakness within minutes. Upon admission, the vital signs and breathing pattern became stable without evidence of anaphylaxis. After magnetic resonance imaging evaluation, the patient was diagnosed with acute ischemic stroke in the right pons, and cerebral angiography revealed moyamoya disease. Reports regarding an allergic reaction without anaphylaxis causing a stroke were extremely limited; however, no study has reported that allergy can cause a stroke in patients with moyamoya to date. Therefore, an ischemic stroke may occur in a patient with moyamoya only with an allergic reaction considered and reported as something that should be considered significant in the daily routine and medication for a patient with moyamoya.
INTRODUCTION
Moyamoya disease is characterized by progressive peripheral stenosis of the internal carotid artery (ICA) and its proximal branches and can cause both ischemic and hemorrhagic strokes1). However, its underlying pathophysiology has not yet been fully elucidated, and this poor knowledge reflects the uncertainty and heterogeneity of patient management2). To date, no pharmacological treatment has been found to reverse the gradual loss in the ICA. Antiplatelet agents are commonly prescribed for ischemic moyamoya disease, although the coexistence of bleeding risk should be considered3).
Allergy-induced anaphylactic reactions can result in vasodilation, hypotension, bronchospasm, and angioedema, and are characterized by a rapid onset of respiratory and circulatory disturbances4).This can lead to cerebrovascular collapse; however, such cases are rarely reported5). In this case report, an allergic reaction was found to result in an ischemic brainstem stroke in patients with moyamoya disease and poor cerebrovascular conditions, although they are not anaphylactic conditions.
CASE REPORT
This 69-year-old patient, despite knowing her peach allergy, developed urticaria on her back and left sided weakness after eating peaches, and presented to the emergency room. On admission, the blood pressure and pulse rate were 136/86 mmHg and 79 beats per min, respectively. On the first arterial blood gas analysis, the partial pressures of oxygen and carbon dioxide were 78.0 mmHg and 38.0 mmHg, respectively. Although the patient had diabetes as an underlying disease, the blood glucose level was 154 mg/dL. The skin had urticaria in the form of red rashes on the back, which were neither pale nor cold. The Glasgow coma scale score was 14 and hemiparesis was found on the left side of grade IV.
Brain computed tomography scan showed no hemorrhagic findings, and brain magnetic resonance imaging scan showed acute ischemic stroke with high-signal intensity in diffuse-weighted images and low-signal intensity in apparent diffusion coefficient in the right pons (Fig. 1).
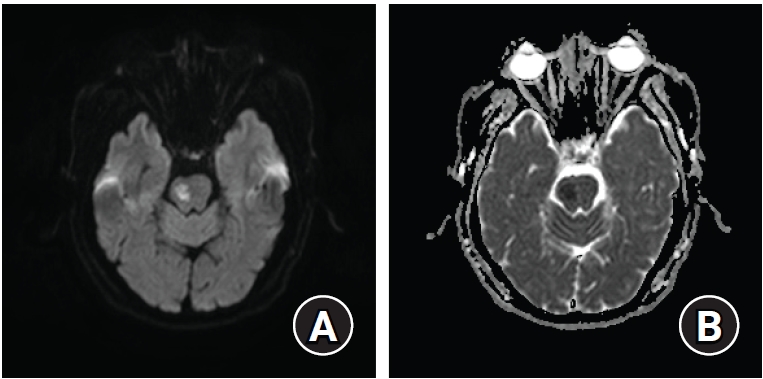
(A) Diffusion-weighted magnetic resonance image shows high signal intensity on the right pons. (B) Apparent diffusion coefficient shows low signal in the same area.
On the magnetic resonance angiography image, both middle cerebral arteries were occluded (Fig. 2), and moyamoya disease with bilateral distal ICA occlusion and collateral circulation from the neovascular structure and external carotid artery branch was confirmed through conventional angiography (Fig. 3).
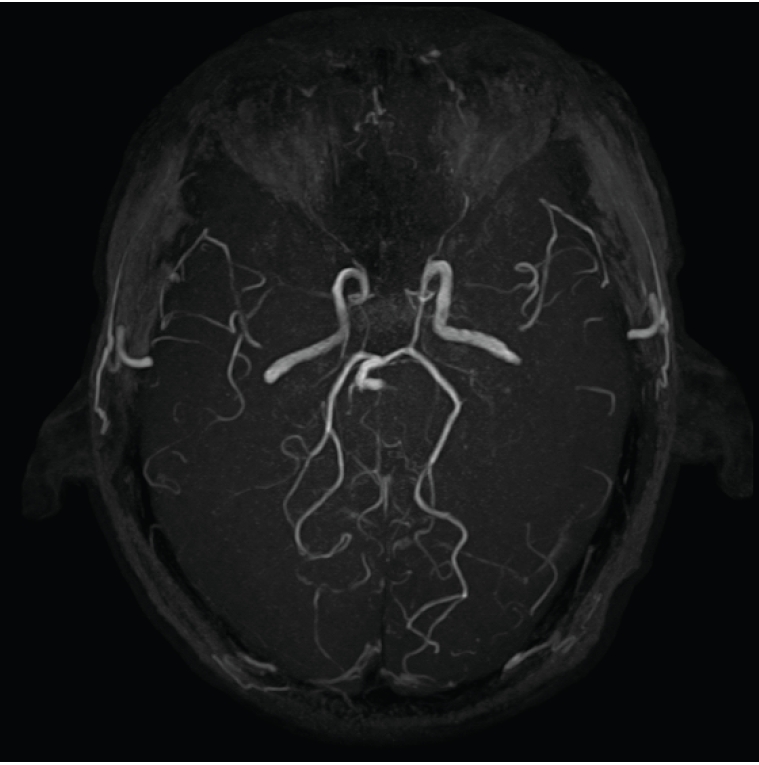
In the magnetic resonance angiography, both distal ICAs were occluded. Also both anterior cerebral arteries and middle cerebral arteries were disappeared.

(A, B) In the cerebral angiography, the moyamoya blood vessels in the form of "puff of smoke" are visible in the both middle cerebral artery territories. (C) Both posterior cerebral arteries form collateral circulation to the both cerebral hemisphere.
The patient was treated with dual antiplatelet therapy with aspirin and clopidogrel and is undergoing physical rehabilitation therapy.
DISCUSSION
Ischemic stroke rarely occurs after a bee sting or drug-induced anaphylaxis, but a few such cases have been reported5,6). However, the cause of ischemic stroke can be easily predicted based on a simple allergic reaction without anaphylactic shock due to a poor cerebrovascular supply caused by moyamoya disease. Despite posterior circulation involvement in moyamoya disease has not been well studied, it is likely an extension of the stenotic process from the anterior circulation7). The allergic reaction may be caused by transient broad peripheral vasodilatation and collapsed fragile cerebrovascular network.
Additionally, an allergic reaction possibly causes autonomic dysfunction8), which result in transient hypotension and ischemic stroke and can also be a means to rationally explain the developmental process9).
The prognosis of moyamoya disease can lead to contradictory results of hemorrhagic or ischemic stroke; however, no methods have been able to predict it yet3).
CONCLUSIONS
This case report intended to provide evidence that an allergic reaction without anaphylaxis can cause ischemic stroke in patients with moyamoya disease, which is considered to be a significant point for both patients and neurologists.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.