Delayed Occurrence of CSF Oculorrhea after Mild Blunt Traumatic Head Injury
Article information
Abstract
Cerebrospinal fluid (CSF) oculorrhea is very rare after traumatic head injury. CSF fistula can cause hazardous complications including infection of central nervous system(CNS). A 40-year-old male visited with epiphora occurring every morning. He underwent traumatic head injury about a year and a half ago. Intrathecal Gadolinium-Enhanced Magnetic Resonance (MR) Cisternography was performed to diagnose his CSF oculorrhea. The delayed CSF oculorrhea was successfully treatment with continuous lumbar drainage. This case report discusses the diagnosis and treatment of the very rare case of the delayed CSF oculorrhea after mild blunt traumatic head injury.
INTRODUCTION
Cerebrospinal fluid (CSF) fistula is an uncommon but well-documented phenomenon which occur after head trauma, typically manifesting as otorrhea or rhinorrhea2,5). CSF rhinorrhea and otorrhea are relatively common complications of head injuries to compare with CSF oculorrhea5). Although it is rare, CSF could enter the orbit following a anterior cranial fossa injury and CSF can exit via the eye, mimicking tear formation10).
The paucity of reported CSF oculorrhea cases, especially compared with the frequency of other types of CSF fistulas developing after traumatic head injury, suggests that cranio-orbital fistulas are rare and may be underdiagnosed complications8).
CSF fistula can cause hazardous complications including infection of central nervous system(CNS), intracranial hypotension, seizures, etc1,8). Therefore, early detection and treatment is required. But CSF oculorrhea is very rare1,3,5,6,9) and it is difficult to diagnose early, because it need to differentiate CSF oculorrhea from excessive lacrimation caused by orbital soft tissue trauma or epiphora caused by lacrimal outflow obstruction2,8).
Therefore, any patient who presents with excessive posttraumatic drainage through the orbit should be suspected to have CSF oculorrhea9).
In this report, the diagnosis and management of one rare case of delayed CSF oculorrhea after mild blunt cranio-orbital trauma is discussed.
CASE REPORT
On October 5, 2018, a 40 years-old male who underwent traumatic head injury about a year and a half ago, visited our outpatient department. The patient complained of epiphora occurring every morning. In glucose stick test at local medical center, blood sugar level has been checked 110mg/dl, and tear's sugar had been checked 68mg/dl. Under suspicion of CSF leakage, the patient was admitted for a thorough examination.
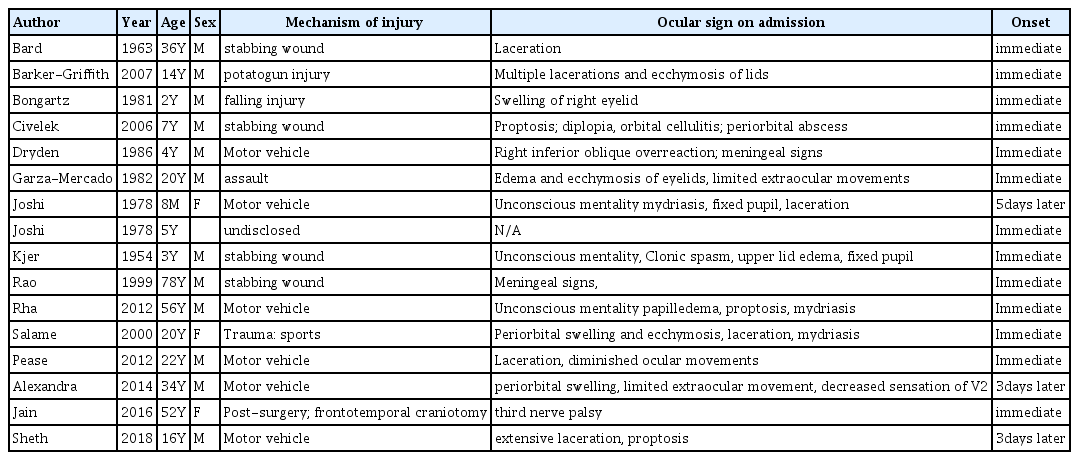
In his past history, there was a car accident against truck on the highway on February 25, 2017. The traumatic epidural hematoma(EDH) and subdural hematoma(SDH) with a linear skull fractures (lateral wall of left sided orbit, temporal, and sphenoid bone) was revealed in his craniofacial computerized tomography(CT) scanning (Fig. 1) but the amount of these hematoma was only scanty and conservative management was done.
Craniofacial computed tomography. A. Axial view shows fracture involving right ethmoid bone(arrow) and lateral orbital wall fracture(arrowhead). B. Coronal view show comminuted fracture involving right frontal bone extent into orbital roof(arrow) and maxillary sinus(arrowhead).
Although the patient suffered from left sided facial paralysis and otorrhagia, due to left sided temporal bone fracture. These symptoms were improved gradually and in the end, there was no CSF leak at the time of discharge.
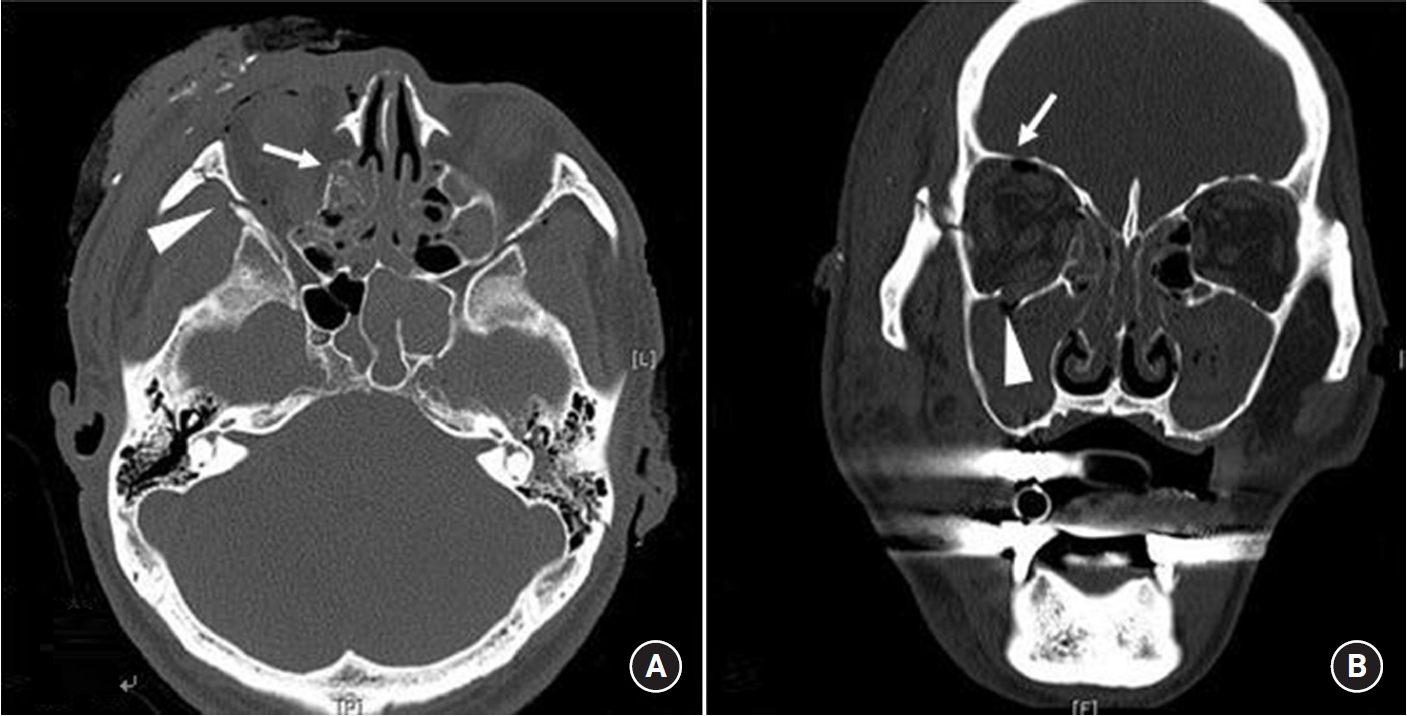
Based on the patient's past history and the glucose level of the eye drop, the CSF oculorrhea was suspected strongly. To confirm CSF leak, Intrathecal Gadolinium-Enhanced Magnetic Resonance (MR) Cisternography (Fig. 2) was performed and CSF collection was identified in inferior part of both orbits and nasopharynx with unidentified fistula site in MRI findings. In spite of conservative treatment with absolute bed rest, CSF oculorrhea was persisted, and we performed continuous lumbar drainage and it was maintained for two weeks.
Intrathecal Gadolinium-Enhanced MR Cisternography. Axial A and Coronal B T1W1 immediately following the intrathecal demonstrate early partial enhancement(arrow). Axial C and Coronal D T1W1 following a 24h delay shows retention of contrast media in inferior part of both orbits and nasopharynx(arrow).
The lumbar drainage catheter removed in two weeks and there was no more CSF leakage during the hospitalization and there were no complications such as cerebral meningitis either. After he discharged, the patient visited our outpatient department 2 weeks and 6 weeks later and there was no CSF leakage any more.
DISCUSSION
CSF leakage typically occurs at four anatomical locations, which is the frontal sinus, the cribriform plate and ethmoid roof, the sphenoid sinus, and the petrous bone8,9), and it occurs due to the defect of anatomical barriers (the skin or mucosa of the air sinuses, the periosteum, the skull bones, the dura mater, and the arachnoid membrane)8,9). When CSF leakage occurred after head trauma, two thirds of the cases occurred within the first 48hours, and the most cases, the leakage detected within 3months8).
CSF otorrhea (CSF leaks through the temporal bone or mastoid fracture associated with dural tears into the middle ear), and CSF rhinorrhea (CSF leaks through fracture of cribriform plate associated with dural tears into the paranasal sinuses and nasal cavity)2) occur commonly, because of a relatively high-pressure gradient between the intracranial space and the external ear canal or paranasal sinuses2). But CSF oculorrhea is rare, because of the relative low pressure gradient between the intracranial subarachnoid space and the intraorbital space2).
In the history of oculorrhea, a case of profuse CSF drainage through the orbit following avulsion of the eye was documented first by Walsh and Hoyt9). And tear like-CSF leakage have been described by Joshi KK, Crockard HA7). The CSF leakage through the orbit was termed ‘oculorrhea’ by Salame K et al.9)
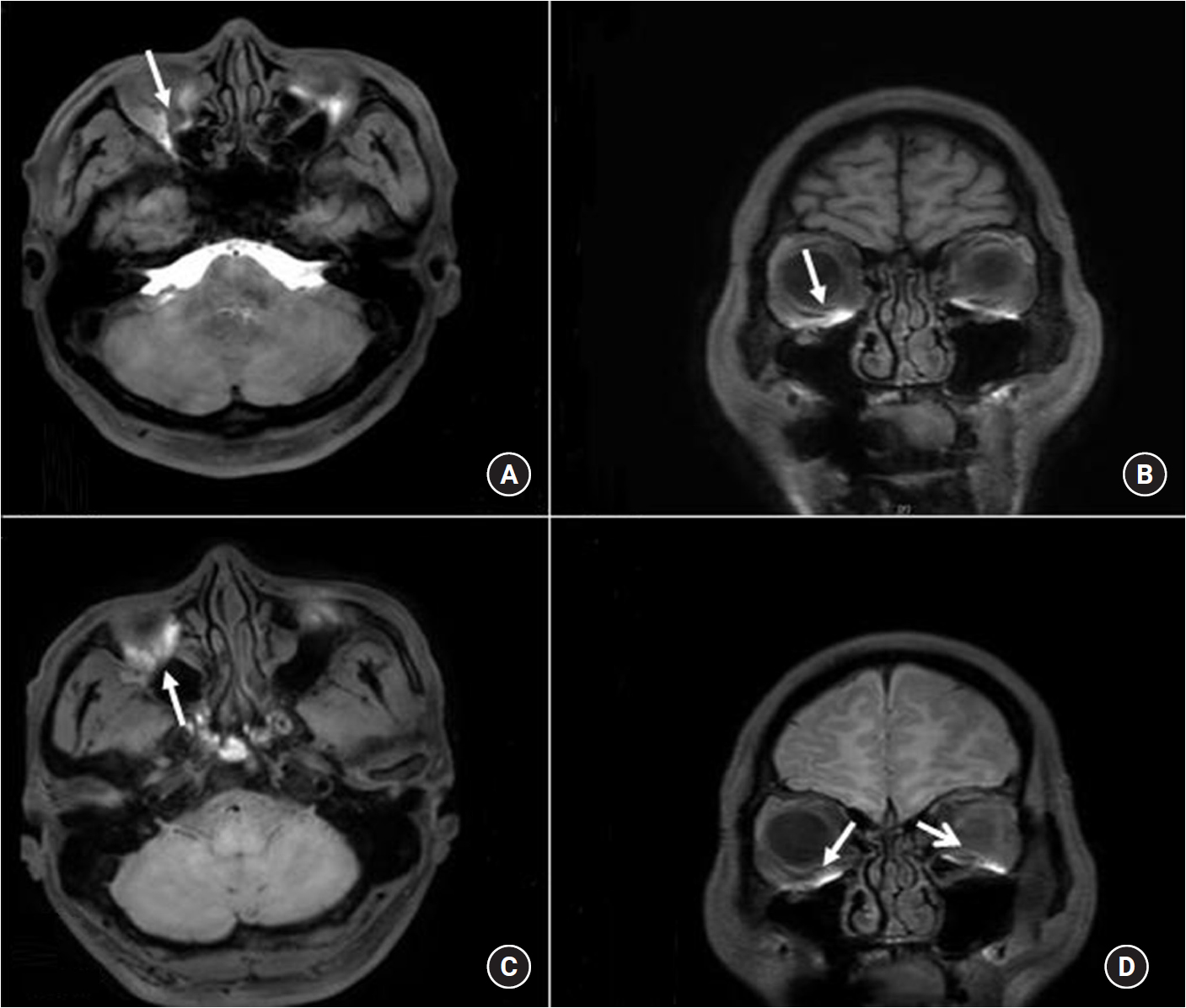
In the reported 16 case of the oculorrhea2,4,8,9,10)(Table 1). It occurred in the relative young ages by severe traumatic head injury within a week after traumatic head injury.
In our case, the patient was a 40 aged-man and he underwent mild blunt head trauma compare with other reported cases. In addition, it was detected in delayed period after trauma.
The delayed CSF oculorrhea can be explained by the persistent fistula between the cranium and orbit10), but to establish the diagnosis of cranio-orbital fistula can be challenging because of the difficulty in differentiating oculorrhea from excessive lacrimation caused by orbital soft tissue trauma or epiphora caused by lacrimal outflow obstruction2).
Delayed CSF oculorrhea should be concerned for all patients with excess tearing after anterior skull fractures8). Because it is difficult to know exactly when it happened. If the CSF oculorrhea detection is missed, the number of complications could be happen and the prognosis of patients should be poor1,8). Therefore we should be suspect CSF oculorrhea in patients with eye drops who has the past history of skull base fracture especially frontal or orbital roof even it is only mild blunt injury8), and if the CSF oculorrhea is suspected, the diagnosis should be done immediately thorough examination and active management is required9).
In the diagnosis of CSF oculorrhea, the analysis of the fluid for glucose concentration may be helpful4,8,9) and Immunoassay for beta 2–transferrin is more specific and requires only a small amount of fluid8,9). CT cisternography with iopamidol followed by thin-sectioned coronal-view CT scanning through the bone window is the best method for localization of the fistula8,9). As in our patient, Intrathecal Gadolinium-Enhanced MR Cisternography can perform in the evaluation of CSF leakage1,3,5).
In most case, the initial management of CSF leak is conservative treatment8,9). However, the rate of complications can increase in cases of delayed CSF oculorrhea, so active treatment is needed. It is important to preventing CSF leak through cranio-ocular fistula and to reduce at risk for infection within the central nervous system2,8,9). We suggest that CSF diversion is proper method for the management of a traumatic cranio-orbital fistula6). CSF diversion can be performed continuous lumbar drainage for up to 10 days10). In spite of continuous lumbar drainage, if the CSF continues to leak, a surgical approach can be taken to primarily repair the dural defect8,10).
CONCLUSION
CSF leakage requires early diagnosis and early treatment, because it can cause serious complications4). CSF oculorrhea is very rare1,3,5,6,9). But, CSF leakage like tears can be occur in patients which is middle-aged man with trauma history even mild blunt head injury especially in the morning. We should be alert in early diagnosis of CSF leakage and immediate and adequate treatment is needed4).
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.