The Latest Classification of Epilepsy and Clinical Significance of Electroencephalography
Article information
Abstract
The classification of epilepsy is revised in 2017, of which framework supports detailed semiology of seizure as well as etiology of epilepsy. Accordingly, there are terms used previously have changed, and new terms that did not exist before. Electroencephalography is indispensable in the diagnosis of epilepsy, and it is also an important way to investigate cerebral activity. In this review, we summarize the classification of epilepsy and discuss the clinical significance of electroencephalography.
INTRODUCTION
Epilepsy is a disease with a history of thousands of years, and it is a functional brain disease that shows various aspects. So far, various efforts have been made to classify epilepsy, and a new classification was announced in 20175,8). In the diagnosis and classification of epilepsy, electroencephalography occupies a very important position. Also, electroencephalography is an essential tool for evaluating the state of the brain due to the nature of the organ (i.e., the brain is ever-changing and it is hard to see its parenchyma with the naked eye).
THE DEFINITION OF EPILESPY AND SEIZURE
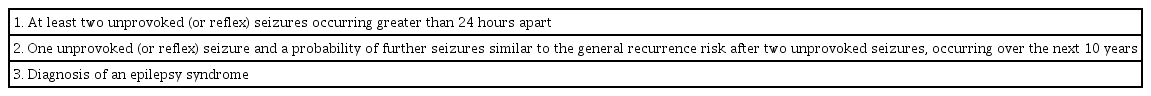
The definition of epilepsy is ‘a group of neurological disorders characterized by epileptic seizures’4). An epileptic seizure is ‘a transient occurrence of signs and/or symptoms due to abnormal synchronous neuronal activity in the brain’6). According to the International League Against Epilepsy (ILAE) official report in 2014, epilepsy should be considered in any of the following conditions: two or more seizures occurring >24 hours apart, one unprovoked seizure and a probability of recurrent seizure risk over 60%, and diagnosis of an epilepsy syndrome (Table 1)4). If there is any epileptiform discharge on electroencephalography, or a potential epileptogenic structure on brain imaging, the probability of recurrent epileptic seizure exceeds 60%2). In addition, the ILAE official report in 2014 re-defined epilepsy as a disease, and suggested a concept of resolved epilepsy. Epilepsy is considered to be resolved if the epileptic is now past the applicable age, or has remained seizure-free over a decade despite a 5-year interruption of anticonvulsant treatment. However, ‘resolved’ and ‘remission or cure’ are not entirely equivalent.
ELECTROENCEPHALOGRAPHY
The diagnosis of epilepsy is unpalatable, and not straightforward. In addition, misdiagnosis is not entirely avoidable7). Although a detailed witness account of the paroxysmal event by a witness is the most important factor for diagnosis, but these testimonies cannot be heard or witnessed in many cases. Thus, electroencephalography is the most important diagnostic test in evaluating a patient with possible epilepsy. It can provide support for the diagnosis of epilepsy and also assists in classifying the underlying epileptic syndrome. As neuro-imaging is advanced for several decades, there is an opinion which underestimates the importance of electroencephalography. However, electroencephalography is highly valuable not only for diagnosis of epilepsy but also for various clinical situations including evaluation of altered mentality, managing patients in neuro-intensive care unit, and intraoperative monitoring. Electroencephalography consists of spatial and temporal summations of postsynaptic potentials generated from a large population of pyramidal cells. The rhythm of electroencephalogram can be defined as the regular appearance of waveforms with similar shapes and comparable periods. Electroencephalography exhibits continuous waves with changing frequency, and it is in good agreement with the patient’s consciousness state. The interpretation of EEG requires the analysis and judgment of the followings: waveform, frequency, amplitude, distribution, rhythmicity, phase relation, timing, persistence (or amount), and reactivity3). It is important that a normal EEG cannot exclude epilepsy. It is also important to note that most abnormal EEG findings are non-specific. Interictal epileptiform discharges are specific finding for diagnosis of epilepsy; rare in normal subjects, but it can sometimes appear. An electroencephalography without abnormal findings are read as normal, however, normal electroencephalography do not necessarily mean ‘the brain is normal’. Electroencephalography reflects the activities and functions of brain cells with high temporal resolution, but it varies greatly depending on the patient’s level of consciousness, sleepiness, the level of sleep, and the drugs used. It is necessary to know the pros and cons of the electroencephalography itself, and to maintain the reading ability by steady efforts.
THE CLASSIFICATION OF EPILEPSY
Classification of the epilepsies has evolved since 1960s1). The latest classification of epilepsy provides a framework for classification of epilepsies8). The framework consists of seizure types, epilepsy types, epilepsy syndromes, and etiology.
The Types of seizure
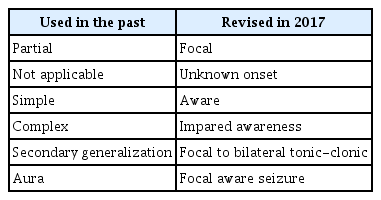
Seizure type is classified by the initial manifestation: generalized, focal, and unknown. ‘Unknown’ stands for a situation when the onset is unknown but other manifestations are known. The term ‘partial’ is replaced by ‘focal’ and is no longer used. As the level of ‘consciousness’ is a vague term, it is replaced by level of ‘awareness’. It is classified by aware (old term simple), and impared awareness (old term complex). Thus, the ‘complex partial seizure’ of the old classification has now replaced by ‘focal impared awareness seizure’. The awareness may not be assessed, then, the mention of awareness can be omitted. Since awareness is impared in most generalized seizures, ‘aware’ vs. ‘impaired’ is omitted. The term ‘focal to bilateral tonic-clonic’ is used to replace ‘secondary generalization’. Table 2 presents the examples of changes in the classification of 2017.
The Types of epilespy
The 1989 classification categorized epilepsies as either focal or generalized. Now, this epilepsy classification become broader in scope than it was and integrate the information including imaging, genetics, laboratory tests, prognoses and comorbidities. The 2017 classification retains the concept of focal and generalized epilepsy, but acknowledges that not all epilepsies can be dichotomized into these two categories. Thus, two additional categories have been added: ‘generalized and focal epilepsy’ and ‘unknown’ if generalized or focal epilepsy. The new group of ‘Combined Generalized and Focal Epilepsy’ has been devised in recognition that there are epilepsy syndromes, e.g., Lennox-Gastaut syndrome. The term ‘unknown if generalized or focal epilepsy’ stands for epilepsies with seizures in which it cannot be clearly determined whether onset is focal or generalized, also be used in an individual who presents with a generalized tonic-clonic seizure and normal examination but whose electroencephalography as well as neuroimaging is non-informative.
Epilepsy syndromes
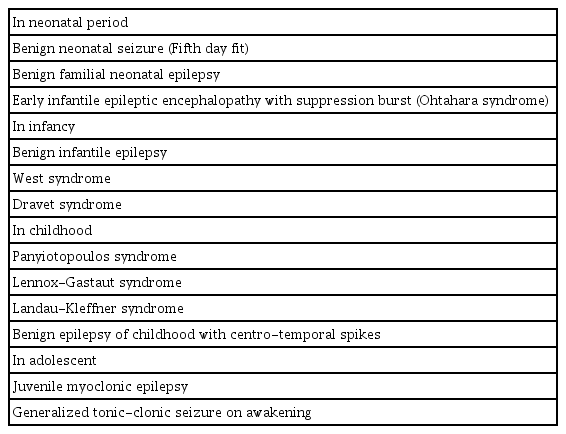
Epilepsy syndromes refer to clusters of features including seizure types, electroencephalographic findings, neuroimaging findings, triggers, and sometimes prognosis. The ILAE has never formally approved or defined a list of epilepsy syndromes, although there have been various well known epilepsy syndromes (Table 3). Epilepsy syndromes tend to be identified in childhood and adolescence. The diagnoses of epilepsy syndrome imply specific information on natural history, comorbidities, intellectual and psychiatric features, applicable management, and prognosis.
Etiology of epilepsy
Not all patients with a specific etiologic diagnosis will have an identifiable epilepsy syndrome. For example, tuberous sclerosis may can manifest as various spectrum of epilepsy. Six etiologies have been defined by the ILAE: structural, genetic, infectious, metabolic, immune, and unknown. These are not hierarchical and more than one might apply.
CONCLUSION
The new classification enable an intuitive grasp, and is transparent for non-clinicians as well. The new classification is designed to cover items not previously classified. The task force of ILAE hope to provide a more practical framework for the classification of epilepsy types, to improve the understanding of seizure and epilepsy.
Notes
No potential conflict of interest relevant to this article was reported.